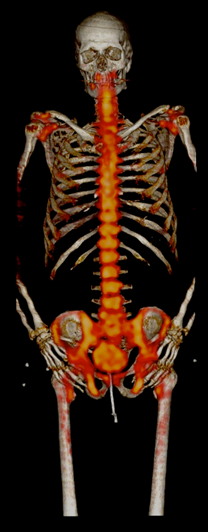
What exactly is a whole-body SPECT-CT?
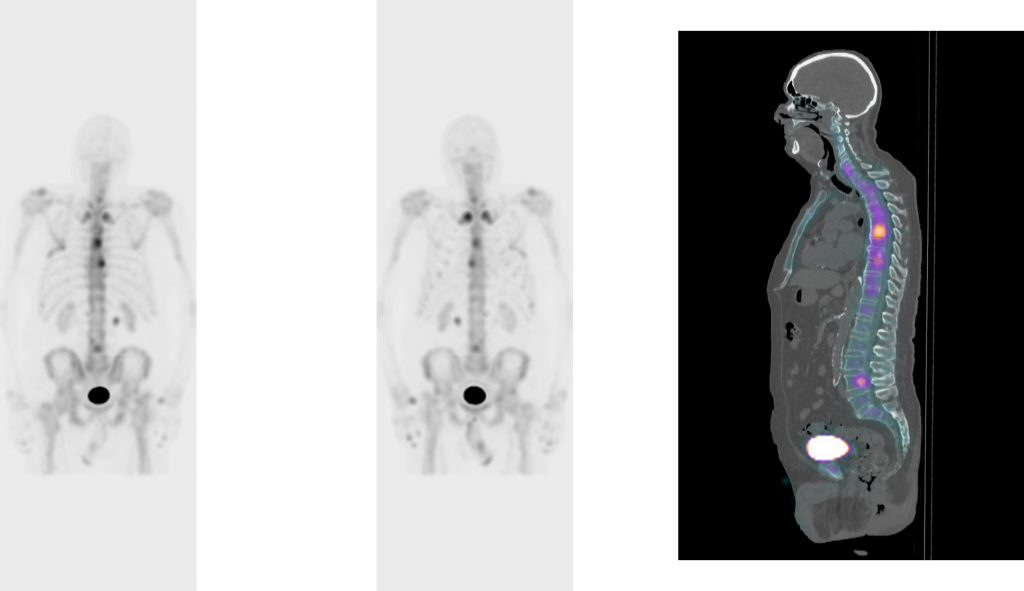
A SPECT-CT scan combines the high sensitivity of a bone scan with the increased specificity of a CT scan. The SPECT-CT study improves the localisation of bone uptake and helps characterise the cause of the bone uptake more clearly. This helps improve the diagnostic accuracy of the bone scan.
“Whole-body SPECT/CT is the optimal modality of choice for metastatic workup, including detection of extra-axial lesions.”
Rager et al. BioMed Research International. Volume 2017
The two sets of three-dimensional images are produced in one sitting and the scans are fused together so that we can correlate the findings on the bone scan with the CT.
A whole-body SPECT-CT consists of multiple SPECT-CT scans “stitched” together to create a continuous image from the head to the toes. In practice it is sufficient to cover from the head to the thigh region. In any case, it is performed in one sitting in a hybrid SPECT-CT scanner.
Modern SPECT-CT scanners with resolution recovery software can perform a whole-body SPECT-CT in a little over 30 minutes, and those with solid state detectors, can be even faster. For instance in a paper by Zacho HD et al. the authors compared the performance of a standard SPECT acquisition of 11 mins with an ultra fast SPECT acquisition of under 3 minutes. They found no significant difference in observer agreement between the two scans.

Why perform a whole-body SPECT-CT?
Traditional bone scans are performed in nuclear medicine departments across the world and are often used to stage malignancies such as lung cancer, breast cancer and prostate cancer. However, although bone scans can be sensitive for bone metastases, they are often poorly specific. There are multitudes of mimics of metastatic disease such as degenerative joint disease, benign bone lesions and artefacts that can mislead even the most experienced radiologist. As a result, many scans are reported with equivocal findings and further examinations are required to corroborate the findings from a bone scan. This can lead to further delays in diagnosis, and occasionally unnecessary interventions for the patient.
Whole body SPECT-CT reduces the equivocal rate of bone scans and improves the diagnostic accuracy.
Löfgren et al. J Nucl Med August 10, 2017
Also, bone scans are not as sensitive for ‘osteolytic’ metastases such as breast cancer, renal cell carcinoma and lung cancer. Often bone metastases from these tumours are ‘lytic’, meaning that they present with holes in the bone. Bone scans are good at detecting osteoblastic metastases, where there is increased bone turn over, but are notoriously poor at identifying osteolytic metastases. This leads to missed diagnoses, and the need to combine a bone scan with other imaging modalities, particularly when osteolytic metastases are a possibility.
In a study by Palmedo et al. (EJNMMI,2014), SPECT-CT has, “a significant effect on clinical management because of correct downstaging and upstaging, better definition of the extent of metastases, and a reduction in further diagnostic procedures.” The authors described an increase in sensitivity of detection of bone metastases from 93.0% with planar bone scanning to 97.2% with whole body SPECT-CT. However, they found a much larger increase in specificity from 78.8% with planar bone scanning to 97.4% with whole body SPECT-CT. They also found that 32.1% of patients were downstaged from a metastatic or suspicious status to a non-metastatic status and 1.5% of patients were upstaged from non-suspicious to metastatic with the use of whole body SPECT-CT.
Other studies have looked at comparing one-bed position SPECT-CT with whole body SPECT-CT. In a paper by Guezennec C et al. the authors compared the whole body planar with single bed position SPECT-CT and a double-bed position SPECT-CT. They found that there was a small incremental improvement in lesion detection with double-bed position SPECT-CT. However, Rager et al. found a more convincing argument for whole body SPECT-CT. They compared planar bone scans with a single SPECT-CT and whole body SPECT-CT. They found that the sensitivity improved from 88.4% with single SPECT-CT to 100% with whole body SPECT-CT and specificity increased from 95.9% to 96.4%.
Radiation Doses
We compared the absorbed doses from our whole body CTs (from vertex to thighs) with the proposed National Diagnostic Reference Limits as described by Iball GR et al. in 2017. We found that our whole body CT dose was similar to the whole body CT dose recommended for PET-CT. Find out more
It is worth noting that we use the maximum injected activity advised by ARSAC for SPECT imaging which is 800MBq compared to 600MBq for planar imaging.
Vertex to thighs
Most CT components that are available with SPECT-CT scanners have a limited table length and usually cannot scan more than 140-160cm. Therefore it is not always possible to perform a SPECT-CT scan from vertex to toes. However, when we look at other staging scans for cancer, such as 18F-FDG PET-CT these studies are usually performed from skull base to mid thighs. In our institution we perform SPECT-CT from vertex to mid thighs and include planar static imaging of the lower legs. We have previously audited the results and found that only in one case of prostate cancer did we find metastatic disease in the lower legs, and in this one patient, they already had widespread metastatic disease throughout the rest of the skeleton that was identified on SPECT-CT. In other words, it is safe to exclude the lower legs when performing staging SPECT-CT scans from vertex to thighs. Find out more
Patient experience
From a patient’s perspective, the scan takes slightly longer than planar imaging. However, there is no need to take additional views after the scan is complete. The patient can be positioned with their arms down and typically the scan lasts 36 minutes. This is usually very well tolerated by all our patients and we have not come across a situation in which a SPECT-CT needed to be abandoned due to patient compliance.
From a technologist’s perspective there is improved patient flow with less need to change the patient positioning or acquire additional views. Find out more
In summary, whole body SPECT-CT improves diagnostic accuracy compared to planar imaging, improves patient care by reducing the false positive rate of planar bone scans and gives a small improvement in sensitivity.
References
- Alqahtani MM, Fulton R, Constable C, Willowson KP, Kench PL. Diagnostic performance of whole-body SPECT/CT in bone metastasis detection using. Clin Radiol. 2020;75(12):961.e11-.e24.
- De Leiris N, Leenhardt J, Boussat B, Montemagno C, Seiller A, Phan Sy O, et al. Does whole-body bone SPECT/CT provide additional diagnostic information over [18F]-FCH PET/CT for the detection of bone metastases in the setting of prostate cancer biochemical recurrence? Cancer Imaging. 2020;20(1).
- Dyrberg E, Larsen EL, Hendel HW, Thomsen HS. Diagnostic bone imaging in patients with prostate cancer: patient experience and acceptance of NaF-PET/CT, choline-PET/CT, whole-body MRI, and bone SPECT/CT. Acta Radiol. 2018;59(9):1119-25.
- Dyrberg E, Hendel HW, Løgager VB, Madsen C, Pedersen EM, Zerahn B, et al. A prospective study determining and comparing the diagnostic accuracy of fluoride-PET/CT, choline-PET/CT, whole-body bone SPECT/CT and whole-body MRI for the detection of bone metastases in patients with prostate cancer. European Journal of Hybrid Imaging. 2018;2(1):19.
- Fleury V, Ferrer L, Colombié M, Rusu D, Le Thiec M, Kraeber-Bodéré F, et al. Advantages of systematic trunk SPECT/CT to planar bone scan (PBS) in more than 300 patients with breast or prostate cancer. Oncotarget. 2018;9(60):31744-52.
- Guezennec C, Keromnes N, Robin P, Abgral R, Bourhis D, Querellou S, et al. Incremental diagnostic utility of systematic double-bed SPECT/CT for bone scintigraphy in initial staging of cancer patients. Cancer Imaging. 2017;17(1):16.
- Iball GR, Bebbington NA, Burniston M, Edyvean S, Fraser L, Julyan P, et al. A national survey of computed tomography doses in hybrid PET-CT and SPECT-CT examinations in the UK. Nucl Med Commun. 2017;38(6):459-70.
- Jambor I, Kuisma A, Ramadan S, Huovinen R, Sandell M, Kajander S, et al. Prospective evaluation of planar bone scintigraphy, SPECT, SPECT/CT, 18F-NaF PET/CT and whole body 1.5T MRI, including DWI, for the detection of bone metastases in high risk breast and prostate cancer patients: SKELETA clinical trial. Acta Oncol. 2016;55(1):59-67.
- Löfgren J, Mortensen J, Rasmussen SH, Madsen C, Loft A, Hansen AE, et al. A Prospective Study Comparing. J Nucl Med. 2017;58(11):1778-85.
- Mavriopoulou E, Zampakis P, Smpiliri E, Spyridonidis T, Rapti E, Haberkorn U, et al. Whole body bone SPET/CT can successfully replace the conventional bone scan in breast cancer patients. A prospective study of 257 patients. Hell J Nucl Med. 2018;21(2):125-33.
- Mostafa R, Abdelhafez YG, Abougabal M, Nardo L, Elkareem MA. Two-bed SPECT/CT versus planar bone scintigraphy: prospective comparison of reproducibility and diagnostic performance. Nucl Med Commun. 2021;42(4):360-8.
- Palmedo H, Marx C, Ebert A, Kreft B, Ko Y, Türler A, et al. Whole-body SPECT/CT for bone scintigraphy: diagnostic value and effect on patient management in oncological patients. Eur J Nucl Med Mol Imaging. 2014;41(1):59-67.
- Rager O, Lee-Felker SA, Tabouret-Viaud C, Felker ER, Poncet A, Amzalag G, et al. Accuracy of whole-body HDP SPECT/CT, FDG PET/CT, and their combination for detecting bone metastases in breast cancer: an intra-personal comparison. Am J Nucl Med Mol Imaging. 2018;8(3):159-68.
- Rager O, Nkoulou R, Exquis N, Garibotto V, Tabouret-Viaud C, Zaidi H, et al. Whole-Body SPECT/CT versus Planar Bone Scan with Targeted SPECT/CT for Metastatic Workup. Biomed Res Int. 2017;2017:7039406.
- Zacho HD, Manresa JAB, Aleksyniene R, Ejlersen JA, Fledelius J, Bertelsen H, et al. Three-minute SPECT/CT is sufficient for the assessment of bone metastasis as add-on to planar bone scintigraphy: prospective head-to-head comparison to 11-min SPECT/CT. EJNMMI Research. 2017;7(1).