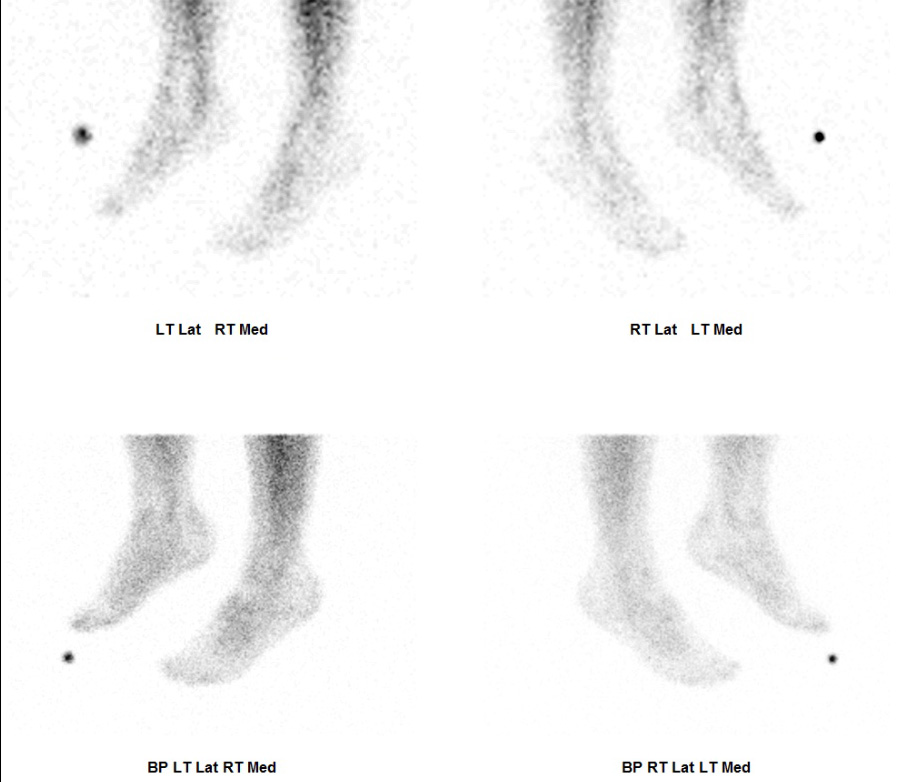
Bloodpool phase imaging is commonly performed as part of a bone scintigram , particularly when we are interested in evaluating prostheses for infection or loosening. The blood pool phase typically follows the dynamic or vascular phase imaging as part of the three phase bone scan. Usually, the blood pool phase imaging is performed at 5 to 10 minutes after the injection of the radiopharmaceutical. Typically, bloodpool phase imaging is performed as a series of static planar acquisitions creating multiple views of a joint.
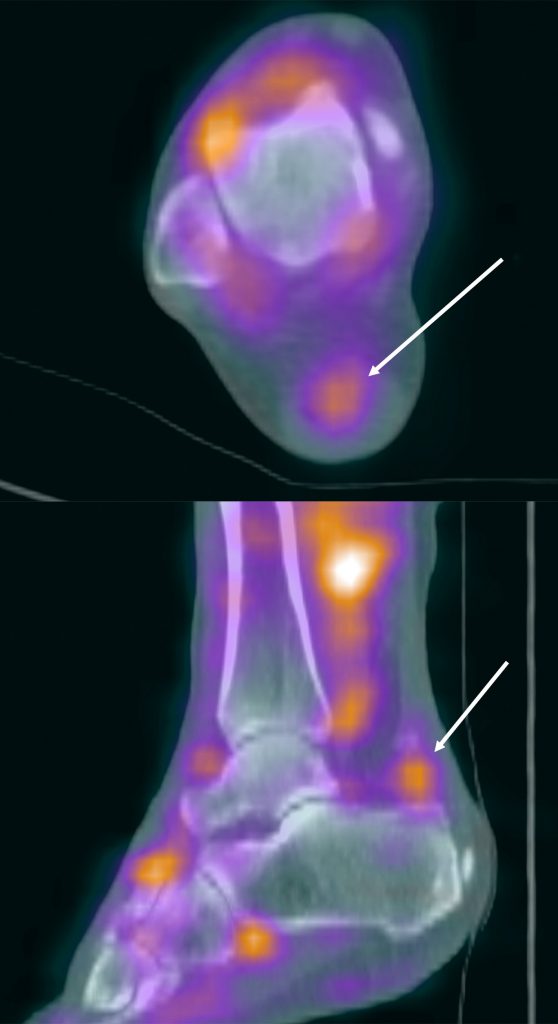
The purpose of bloodpool phase imaging is to assess for hyperaemia and inflammation in the bone or joint. Essentially, the tracer leaves the capillaries due to increased permeability associated with an inflammatory response. The tracer surrounds the extracellular fluid surrounding the osteoblasts, before it is taken up during the delayed uptake phase. In this way the blood pool phase imaging allows us to evaluate for the ‘leakiness’ of the capillaries and highlights sites of active inflammation. Bloodpool phase imaging allows us to appraise for inflammation in the soft tissues as well as the bone. In some cases, it can be difficult to differentiate soft tissue inflammation from bone inflammation on planar imaging. In this case the CT component of the SPECT-CT improves localisation compared to SPECT alone.
Why perform bloodpool SPECT-CT?
Bloodpool phase SPECT-CT imaging allows us to better delineate the sites of increased blood pool phase uptake and can help differentiate soft tissue from bone activity. In a study by Aydogan et al. (1) the authors used bloodpool SPECT imaging to assess the viability of the mandible following mandibular reconstruction. The authors found that SPECT improves the visibility of the increased blood pool activity within this complex anatomical region. The mandible is difficult to image with a planar scan because of its shape and location. In practical terms it is difficult to move the detector close enough to the mandible in order to acquire good image quality. The SPECT acquisition allows visualisation of this complex 3D structure during bloodpool phase and remains comfortable for the patient.
A further study by Phillips et al. (2) looked at assessing the feasibility of a rapid bloodpool SPECT-CT acquisition. They studied a SPECT acquisition using 30 seconds per step with a total SPECT time of less than 4 minutes. They found that the rapid SPECT-CT was feasible and produced accurate blood poolphase images compared to planar bloodpool phase imaging. The authors found bloodpool SPECT-CT helpful in more accurately localising infection and inflammation.
Bloodpool phase SPECT-CT has been useful in identifying soft tissue pathology on bone scans as seen by Cuvilliers (3, 4) et al. who concluded that, “adding bloodpool SPECT- CT to standard three phase bone scans impacted diagnostic conclusion in a quarter of the patients with painful lower extremities, notably by revealing significantly more tendonitis.”
Bloodpool SPECT-CT is useful in assessing patients with painful knee prostheses as investigated by Verschueren et al (5). Bloodpool phase SPECT has better interobserver agreement compared to planar bloodpool phase imaging. The authors noted that, “The use of SPECT improved inter-rater agreement in 81% of assessed areas, and significantly improved rater confidence by 20%. Importantly, statistically significant gains in agreement were observed in 24% of regions, including those that convey clinically relevant information on prosthesis biomechanics and failure modes, such as the superior lateral femoral regions.” The authors also noted that knee prostheses with certain sites of increased activity on bloodpool phase SPECT tended to have a poorer outcome and were more likely to require revision surgery. They were able to suggest that blood SPECT may be able to differentiate local stress from loosening of the component.
This has important consequences for those of us interpreting SPECT-CT scans. Essentially, the presence of bloodpool phase uptake in of itself is shown to be a poor prognostic marker for loosening of the knee prosthesis. The same principle can be applied to imaging other joints. In my experience so far with bloodpool SPECT-CT, I have found that sites of bloodpool phase uptake on SPECT-CT are likely to be significant pain generators. The presence of bloodpool phase SPECT-CT activity can help differentiate pathological uptake from normal bone remodelling. This is important because we know that bone uptake on delayed phase scans can persist for several years and can be a normal finding following surgery or trauma.
In our institution, when performing a three-phase bone scan, we will perform a blood pool phase SPECT-CT immediately after the dynamic / vascular acquisition. We are also currently performing planar bloodpool imaging, but we will soon be omitting this from the imaging protocol once we are accustomed to interpreting the bloodpool SPECT-CT.
My Experience
The bloodpool phase SPECT acquisition consists of 60 frames (6 degrees per frame) at 7 seconds per frame (7 minute SPECT time). The CT component is a low dose CT for attenuation correction and anatomical localization purposes only (80kV with 10-25mAs). Typically, this is a 5 mm slice thickness with a high noise index compared to the diagnostic CT which is performed as part of the delayed phase SPECT-CT scan.
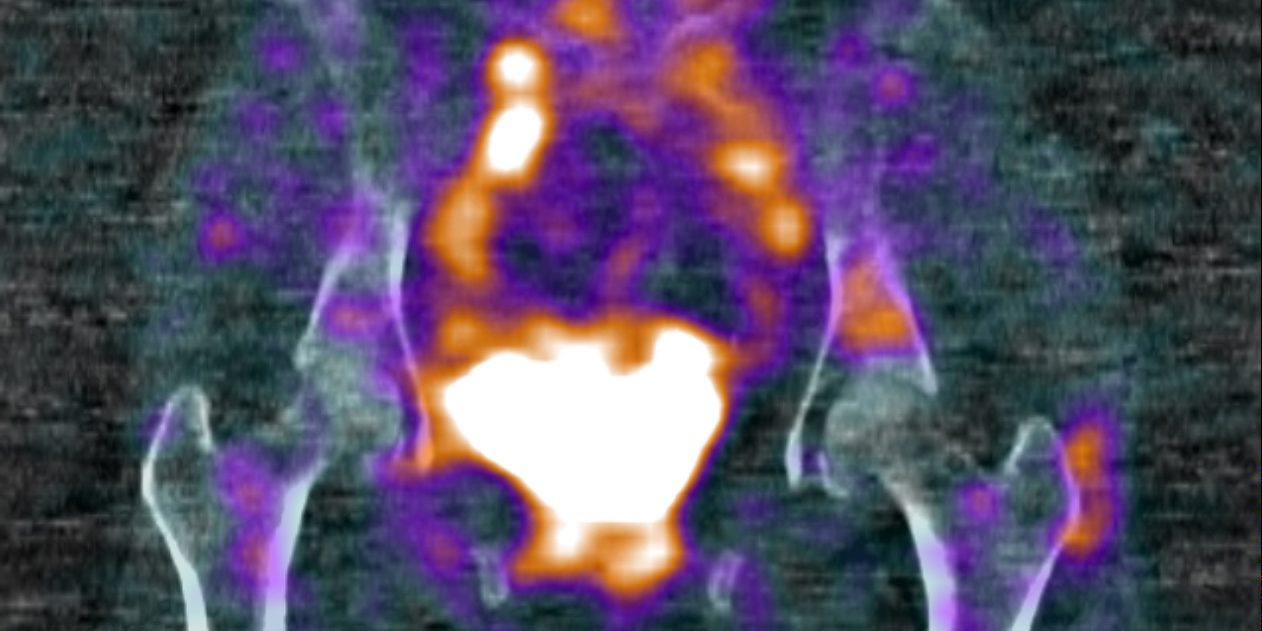
There are several challenges facing us when performing a bloodpool phase SPECT-CT. For instance, the patient may need to be repositioned between the dynamic acquisition and the blood pool phase SPECT-CT. There are also limitations on the camera usage, which can be a problem if you have only one SPECT-CT scanner available in your department. These scans are also trickier to report. Normal bloodpool phase activity needs to be re-learnt, including the normal vascular anatomy. The thresholding of the scans can be difficult when displaying the bloodpool phase due to the intense vascular activity and urinary bladder activity. Often the bloodpool activity in the soft tissues and bone can be low grade and much less intense than the urinary activity. The bloodpool phase SPECT-CT allows us to evaluate the soft tissues as well as the bones when performing a bone scan. Therefore, it is important to know the anatomy well and have a thorough understanding of the musculoskeletal pathology. For instance, we can identify tendinopathy and ligamentous injuries with bloodpool phase SPECT-CT that we would not have previously with planar imaging.
In my experience so far with performing blood spool SPECT-CT, the additional time involved in both acquisition and reporting the studies is beneficial in that it allows us to more accurately identify sites of inflammation and also allows us to diagnose pathology that we would not have seen with standard bone scintigraphy.